CNAO – National Centre for Oncological Hadrontherapy
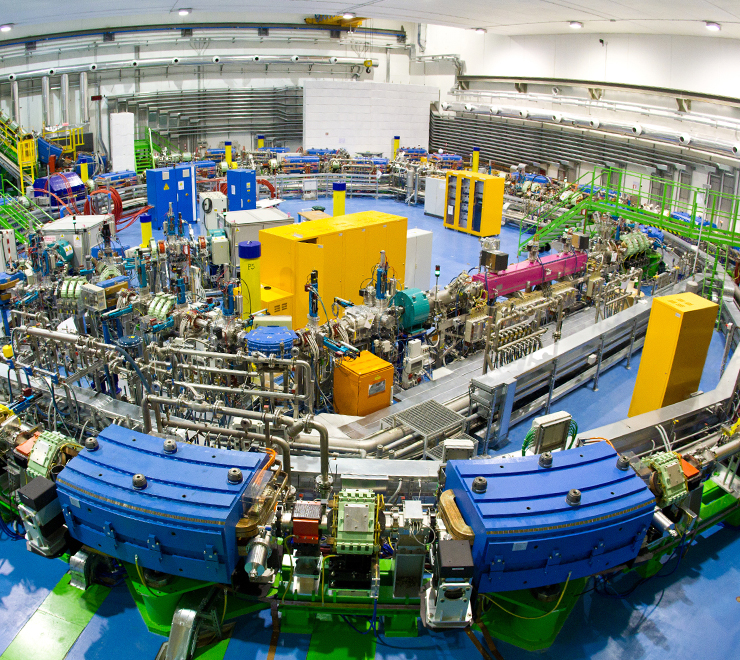
CNAO (National Centre for Oncological Hadrontherapy) is an innovative and technologically advanced clinical facility, established by the Italian Ministry of Health with Law n° 388 of December 23, 2000, for treating radio-resistant or inoperable tumours with carbon ions and protons.
DISCOVER CNAO VIRTUAL TOUR: https://virtualtour.fondazionecnao.it/en/
At CNAO, we treat the following pathologies with hadrontherapy:
- Head and neck sarcomas
- Thoracic Abdominal wall and Pelvic sarcomas
- Sarcomas of the extremities
- Ocular melanoma
- Brain tumours
- Gynecological tumours
- Spinal and paraspinal tumours
- Pediatric solid tumours
- Malignant pancreatic cancers
- Liver primary tumors
- Re-Irradiation (any site)
Head and Neck tumours
Head and neck cancer (HNC) is a rare disease that can affect different sites and is characterized by variable incidence and 5-year survival rates across Europe. Multiple factors need to be considered when choosing the most appropriate treatment for HNC patients, such as age, comorbidities, social issues, and especially whether to prefer surgery or radiation-based protocols.
Given the complexity of this scenario, the creation of a highly specialized multidisciplinary team is recommended to guarantee the best oncological outcome and prevent or adequately treat any adverse effect. Data from literature suggest that the multidisciplinary team-based approach is beneficial for HNC patients and lead to improved survival rates. This result is likely due to improved diagnostic and staging accuracy, a more efficacious therapeutic approach and enhanced communication across disciplines.
Despite the benefit of a multi disciplinar tumor discussion (MTD), it must be noted that this approach requires considerable time, effort and financial resources and is usually more frequent in highly organized and high-volume centers. Literature data on clinical research suggest that patients treated in high-accrual centers report better treatment outcomes compared to patients treated in low-volume centers, where a lower radiotherapy-compliance and worst overall survival have been reported. There is general agreement that treatment of rare cancers such as HNC should be concentrated in high volume, specialized and multidisciplinary centers.
In order to achieve this goal, the creation of international collaboration network is fundamental. The European Reference Networks for example aim to create an international virtual advisory board, whose objectives are the exchange of expertise, training, clinical collaboration and the reduction of disparities and enhancement of rationalize migration across Europe. The purpose of our work is to review all aspects and challenges in and outside this network setting planned for the management of HNC patients.
DISCOVER THE PATIENT’S COURSE HEAD AND NECK DISTRICT
Ocular melanoma
Ocular melanomas are the most common intraocular malignancy in adults. The majority of ocular melanomas are choroidal melanomas. These tumours can be difficult to diagnose, especially when they are small. Documented growth of a lesion on serial examinations is the most important clinical feature favouring the diagnosis of a choroidal melanoma. Diagnostic studies including ultrasonography and angiography may be helpful in the diagnosis of these tumours. A number of treatment options are available for choroidal melanomas. These include photocoagulation, radiation therapy, local tumor resection, and enucleation.
Ocular protontherapy (OPT) is considered the elective treatment for different kinds of highly malignant intraocular tumours like uveal, iris and conjunctival melanomas, ocular hemangioma and retinoblastomas. A remarkable local control rate (well over 90%) has been reported over the years by several institutions.
At CNAO, OPT treatments started in September2016 using a non-dedicated horizontal beamline featuring active scanning delivery.
The standard clinical protocol foreseen a pre-treatment surgical procedure, aimed at implanting radiopaque tantalum clips on the eye globe surface in close proximity to the tumor site. This preparatory procedure is typically carried out by ophthalmologists in hospital facilities that collaborate with CNAO.
Clips are used both during planning and treatment phases as a geometrical reference to identify the target volume and to ensure setup repeatability, relying on X-ray based image guidance procedures. Concerning OPT, the planning phase consists of the acquisition of at least two orthogonal X-ray images while the patient is looking straight forward. This set of images is used to determine the optimal gaze direction (polar and azimuth angles) to minimize the dose to critical structures and achieve total coverage of the target by the prescribed dose.
OPT treatment at CNAO is delivered in four subsequent daily fractions with the patient seated and immobilized on a 6 DoF (degree of freedom) robotic treatment chair. Setup robustness is established via a personalized thermoplastic mask and eyelid retractors, and patient position is verified and iteratively corrected with a point-based rigid registration of radiographic images of the tantalum clips.
A safe and effective irradiation envisages an adequate organ motion mitigation strategy. Throughout treatment, the patient is asked to stare at a fixation light embedded in a custom eye tracking system (ETS) accurately positioned by industrial robots for precisely reproducing the prescribed optimal gaze direction. Stereo cameras embedded in the ETS allow the operators to monitor the gaze direction in real time and guide the beam on/off delivery consequently.
Bone and Soft tissue Sarcomas
Bone and Soft tissue sarcomas are a rare type of malignant tumors that develops in bone and connective tissue, such as fat, muscle, blood vessels and nerves.
There are over 80 different subtypes of sarcomas. They can affect any part of the body and can occur at any age. In general, STS strike in childhood (with specific subtypes), in adults (third and fourth decades) and especially in mature age, after the age of 60. Bone sarcomas predominantly affect adolescents and young adults, although the age group affected varies depending on the type of sarcoma.
Sarcomas, especially in the initial stages, do not present specific symptoms and/or may remain asymptomatic. For this reason, they are often diagnosed late, when the disease is already in an advanced stage and/or has spread to other parts of the body (metastasis).
Before starting any treatment, it is mandatory to obtain a correct histological diagnosis from expert pathologists.
The therapeutic proposal requires an evaluation by a “multidisciplinary group”, i.e. a group composed of different types of specialists, including the surgeon, the medical oncologist and the radiation oncologist, in order to propose to the patient the most appropriate treatment path.
The necessary specialist skills are present in the reference centers, which can be connected to each other and to other oncology centers to form a “dedicated networks”.
Surgery is the main therapeutic option for bone and soft tissue sarcomas when it is carried out in a radical oncological manner through total removal of the tumor “with wide margins”
In case the surgeon evaluates that the tumor is not operable in a conservative way, hadrontherapy with protons or carbon ions can be a valid alternative to X-ray radiotherapy since it has the advantage to deliver higher biological effective dose to these highly radio-resistant tumors while limiting damages to surrounding tissues.
Hadrontherapy can also play a role before surgery (neoadjuvant intent) or after surgery (adjuvant intent).
DISCOVER THE PATIENT’S COURSE THORACO-ABDOMINAL AND PELVIC DISTRICT PATHOLOGIES
Brain and Skull base tumours
Hadrontherapy is particularly effective for certain types of brain and skull base tumours because it allows for precise targeting of the tumour with minimal damage to surrounding healthy tissues. Here are some histologies that can be treated with hadrontherapy:
. Gliomas
• Low-grade gliomas: These slow-growing tumours can benefit from the precise targeting of hadrontherapy.
• High-grade gliomas (Glioblastoma): Though challenging to treat, hadrontherapy can be used to target residual tumor cells after surgery.
. Meningiomas
• These are typically benign tumours arising from the meninges, the layers of tissue covering the brain and spinal cord. Hadrontherapy is useful for tumours located in critical areas where surgical removal is difficult or risky for sequelae.
. Chordomas
• Rare, slow-growing tumours, chordomas belong to the family of bone sarcomas, and can develop in the bones of the skull base and spine. Hadrontherapy is particularly beneficial for chordomas due to their resistancy to conventional radiation therapy and based to its high selectivity and to the possibility to spare the spinal cord and brain stem.
. Chondrosarcomas
• A type of cancer that occurs in the cartilage of the skull base. These tumours are also resistant to conventional radiation, making hadrontherapy a better option.
. Medulloblastomas
• These are fast-growing, high-grade tumours most commonly seen in children. Hadrontherapy can help minimize long-term side effects by reducing exposure to surrounding healthy brain tissue.
. Pituitary Adenomas
• Generally benign tumours that occur in the pituitary gland. Hadrontherapy can target these tumours precisely, sparing surrounding critical structures such as the optic nerves.
. Pediatric Brain Tumours
• Various pediatric brain tumours can be treated with hadrontherapy to minimize long-term side effects on the developing brain.
Gynecological tumours
Gynecological melanomas are rare neoplasia that affect the vulva in 4% of cases, the vagina in 2% and the uterine cervix in less than 1% of cases.
Melanomas of the uterine cervix and vagina are extremely aggressive pathologies, with a usually unfavourable prognosis, and mortality rates of 20-50% 5 years after the tumour is treated.
The treatment of gynaecological melanomas depends on a series of factors, such as the size and location of the tumour, the patient’s age and physical condition. In addition, due to the rarity of these tumours it is difficult to identify an effective therapeutic strategy.
Usually, treating these melanomas involves surgical resection, while if tumours are in an advanced stage, chemotherapy can be used. For cases of particularly hard-to-treat tumours, radiation therapy with carbon ions is considered a potentially effective non-invasive treatment.
In recurrences of gynaecological tumours, hadrontherapy is a potentially effective therapeutic option that permits, thanks to its greater biological efficacy, treating radio-resistant neoplasias as well, sparing the surrounding healthy structures.
Pedriatic solid tumours
The hadrontherapy treatment, in particular with protons, may be useful for the treatment of paediatric solid tumours. For this type of tumours, the main advantage of hadrontherapy is related to the need to preserve healthy tissues avoiding unnecessary irradiation.
In fact, most of the tumours that affect children involve the brain, so the opportunity to better preserve healthy brain tissues is preferable.
Reducing the dose to healthy tissues drastically reduces the risk of developing secondary tumours once children become adults.
Furthermore, in 2025, CNAO will open a new proton therapy area and treatment room equipped with a gantry able to rotate particle beams around the patient. The rotating gantry will be particularly useful for treating pediatric solid tumours, allowing for more precise targeting of the tumor mass.
The clinical documentation regarding paediatric patients and the related requests for treatability with hadrontherapy must be sent to CNAO by the paediatric oncology centre that treats the child, in order to guarantee the continuity of the clinical pathway in a multidisciplinary perspective.
In evaluating the effective clinical advantage of treatment with protons compared to traditional radiotherapy, we are committed to collaborate in a multidisciplinary approach with the most important National and International Oncological centres.
Liver tumours
Primary tumours of the liver and the biliary tract are hepatobiliary neoplasias that can be classified into:
• Liver tumours
• Biliary tract tumours
Among primary malignant liver tumours, the most common one is certainly the hepatocellular carcinoma.
The treatment of hepatocarcinoma varies depending on a number of factors such as the patient’s general medical condition, the stage of the disease, the number of tumour masses present, where they are located, their size and if there any metastases. Therefore, the therapeutic treatment has to be always assessed by a multidisciplinary team.
The therapy of choice is usually surgery, although this approach cannot be often adopted due if the disease is diagnosed when it too advanced (i.e. vessel infiltration)
In selected cases of primary inoperable large hepatocarcinoma hadrontherapy, based on its precision may be a treatment option.
Malignant pancreatic cancers
Different types of tumours can affect the pancreas and the most common is
• Adenocarcinoma: it starts in the ducts that carry digestive enzymes. It grows and spreads quickly, and diagnosing it at an early stage is very difficult. The number of cases in Europe is constantly growing: in Italy more than 10,000 people get this disease every year.
In its early stages, pancreatic cancer is asymptomatic, a characteristic that, unfortunately, can make it difficult to diagnose. The first therapeutic indication in case of pancreatic cancer is surgery.
Hadrontherapy is indicated:
• for selected cases of locally advanced, inoperable pancreatic tumours
There is no indication to hadrontherapy in metastatic cases.
Locally advanced pancreatic tumours are inoperable tumours that have reached large blood vessels; in these cases, chemotherapy cycles is indicated.
Re-Irradiation treatments
Patients with disease recurrence in an anatomical region/district previously undergone to radiotherapy might be considered for retreatment by hadrontherapy.
Recurrent tumors after previous RT are tipically radioresistant disease and may benefit from the high biological effectivesess and physical selectivity of particles.
Details of the previous RT plan in DICOM format are mandatory for treatment evaluation.
fondazionecnao.it
Head and neck tumours
Ocular melanoma
Chordomas and Sarcomas
Brain tumours
Gynecological tumours
Re –Irradiation treatments
Pedriatic solid tumours
Primary tumours of deliver
Malignant pancreatic cancers
ORGANIZATION FIGURES
| RESIDENT DOCTORS | 17 |
| IN-HOUSE NURSES | 7 |
| FULL TIME STAFF | 166 |
| YEARLY PATIENTS | 5000 |
OPENING HOURS
| Monday – Friday | 8:00 – 18:00 |
+39 0382 078306
ADDRESS
Via Erminio Borloni, 1 27100 Pavia
SOCIAL
CONTACT OUR INTERNATIONAL DEPARTMENT
CNAO is the only Centre in Italy and one of the 6 centres in the world able to provide hadrontherapy with both protons and carbon ions for treating the rare tumours. International patients can access hadrontherapy treatments according to the intra-EU mobility rules, bilateral agreements or private health insurances.
OUR PATIENTS SAY
The stories of our patients are very important and help to foster knowledge and increase trust in an innovative treatment such as hadrontherapy.

“Professionalism, Humanity, Family: CNAO in three words.”

“I have met a fantastic team who took care of me during the whole treatment period and made me feel so safe!”

“I had begun to love that amazing machine, that with its beam fought with me and for me.”